Wisconsin Shaken Baby Syndrome What Percent of Perpetrators Are Male
Original article
peer-reviewed
Epidemiology of Calumniating Head Trauma Among Children in Saudi arabia
Abstract
Background and objectives: To examine abusive caput trauma (AHT) trends using information obtained from hospital-based kid protection centers (CPCs) and the distribution of age in months amongst immature children in Saudi Arabia.
Methods: A retrospective study was conducted that includes data obtained from 58 infirmary-based CPCs in all 13 regions of Saudi Arabia registered in the National Family Safety Registry from 2010 to 2020. AHT cases (n=106) were identified for inclusion in the registry by a daily review of the emergency department logbooks.
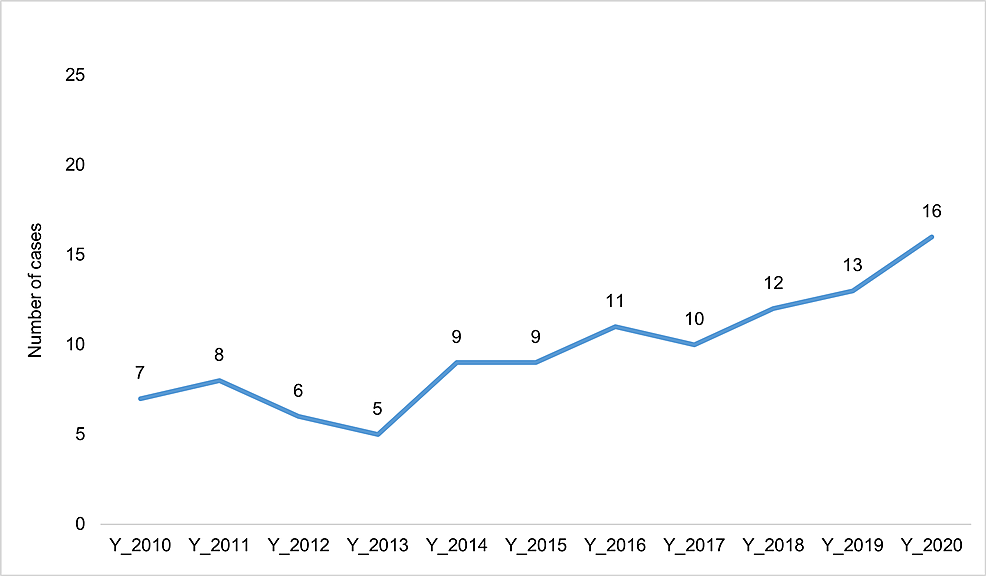
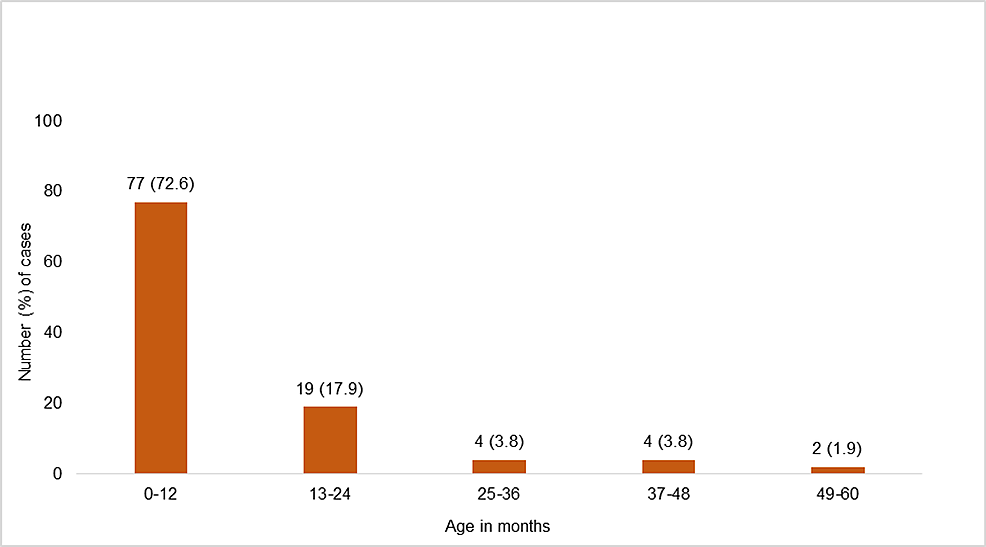
Results: Over the 11-yr menstruation, there was a sharp increase in the number of cases, specifically subsequently 2014, from seven cases per year in 2010 to 16 cases in 2020. AHT affects predominantly children anile 0-12 months (72.vi%), followed by xiii-24 months (17.nine%), 25-36 months (3.8%), 37-48 months (3.8%), and 49-60 months (1.ix%). Victims were characterized past a predominance of crying infants (23.6%), past history of abuse (xiii.2%), a kid'due south chronic disease and disability (7.6%), and prematurity (ii.viii%).
Conclusion: Different grooming and educational programs demand to exist performed to raise awareness of AHT. Enacting the pediatrician's mandatory reporting law will improve the rate of reporting cases.
Introduction
Abusive head trauma (AHT) is the deadliest form of child maltreatment (CM) and is the leading crusade of death among the victims [ane]. In the United States (US), according to the Centers for Affliction Command and Prevention (CDC) [ii], AHT tin be defined equally an injury to the skull or intracranial contents of children <five years due to intentional precipitous impact and/or tearing shaking. Contempo epidemiological studies have identified mothers <eighteen years, mothers with low instruction, male caregivers, caregivers of substance corruption or mental health disorders, single-parent families, families with low socio-economic status, multiple gestations, and non-European American descent as the risk factors for AHT [iii,four]. There are some characteristics among children that appear to increase the probability of AHT including age <1 year, male, and premature birth or low nascence weight [four]. Previous inquiry reported that AHT children - of all severities of injury - have 20% mortality and almost 50% permanent inability rates [5]. The consequences of AHT are severe including learning difficulties, hearing and physical disabilities, cognitive palsy, vision and spoken language problems, seizures, cognitive damage, and decease [half dozen]. Baeesa and Jan reported characteristic signs such equally altered level of consciousness, retinal/intracranial hemorrhages to those who were suspected to have AHT [seven]. Furthermore, the average hospital charge for AHT patients was approximately $xxx,000 [eight].
The incidence of admitted AHT children (per 100,000 children) was reported from 12.5 to 38.8 in many Western countries including the The states (<1 twelvemonth old) [3], United Kingdom (UK) (<2 years old) [9], and Australia (<2 years old) [x]. Nearly 80% of all AHT occurs amid children age <ii years [xi], with infants age <1 yr having an incidence approximately viii times that of two years [3]. According to CDC, the incidence in the United states of america was 0.76 fatal cases of AHT per 100,000 children <4 years, increasing to two.14 when because only children <one yr [12]. In Scandinavian countries, there is a lack of reports from population-based studies in terms of the incidence of AHT [thirteen]. Myhre et al. reported a retrospective case series of infants and toddlers admitted with AHT to a tertiary intensive care unit in Norway [14]. In Sweden, Tingberg et al. conducted a retrospective medical record review of infants presenting to a pediatric emergency department with a caput injury and revealed that 54% identified infants had a history that should accept prompted suspicion of AHT [15]. Another report in Republic of estonia reported an incidence of AHT (28.vii per 100,000) among children ≤1 twelvemonth [sixteen].
Information technology is obvious from the literature review that there is a lack of publications on AHT that have emerged from Middle Eastern countries where children and adolescents comprise a large proportion of the population [17]. A regional study conducted in Bahrain reported that most of the children (78%) were ≤1 yr erstwhile and the mortality charge per unit was 17% [ane]. In Saudi arabia (SA), AHT was kickoff recognized in 1994 [xviii]. National hospital-based registry reported that AHT represents five% of the physical corruption. The suspected perpetrators include males (60%), unemployed, and/or with low levels of education of parents/caregivers. The mortality rate was 25% and near of the surviving children (70%) were discharged with moderate to severe neurological disorders [13].
While in that location are numerous publications of a clinical nature on AHT, few population-based epidemiological studies be that enable to estimate the frequency and identifying its risk factors. Identifying the issue and its characteristics is important to increment awareness and recognition. However, there is little knowledge of such a context in SA making it an surface area in urgent need of exploration. In this study, we report the demographic characteristics, incidence, risk, and outcome for AHT cases in SA.
Materials & Methods
A retrospective report was conducted that includes data obtained from 58 hospital-based Child Protection Centers (CPCs) in all xiii regions of SA registered in the National Family Safety Registry (NFSR) from 2010 to 2020. The NFSR is a web-based online affliction registration organization that collects data from CPCs and Adult Protection Centers within the SA. AHT cases (<5 years) were identified for inclusion in the registry by a daily review of the emergency department logbooks by the suspected child abuse and neglect (Scan) squad - a multidisciplinary team that includes physicians, nurses, and social workers with extensive feel in the management of CM cases.
Information nerveless include demographic characteristics of the children (historic period and gender), information of caregivers and perpetrators, history of previous abuse, and fatality. Descriptive analysis was conducted for the study variables.
All data entry forms have validation checks and alarm messages that restrict users from making whatsoever data entry mistakes. Validation rules are designed every bit a quality check of information entered in the database. The diagnosis validation rules that are integrated are run routinely to ostend accuracy. Since the registry collects personally identifiable health information, one of the major responsibilities of the common user is to ensure attending to privacy equally a central consideration in the collection and maintenance of the information obtained. The NFSR ensures that only authorized individuals should handle the raw data and data managed by the registry database, and is attainable to the advisable people through assigned passwords. After blessing from the NFSR board, registry data are released to the researcher to ensure that the privacy of individuals does not replace other rights or societal goals while carrying out the inquiry.
The study obtained ethical clearance from the Institutional Review Board (IRB) of the King Abdullah International Medical Inquiry Center (KAIMRC) in Saudi Arabia. Hospital medical record numbers were used without whatsoever identification cloth. The data were collected only for research purposes and were not used for other purposes. A series of measures were taken to ensure the protection of confidentiality. The information did non contain the name of the patient but were labeled with a reconstructable personal alphanumeric identifier. All information were stored on a designated computer with an access-limited locked difficult drive.
The study was approved by the Institutional Review Lath (IRB) of the Rex Abdullah International Medical Research Center (KAIMRC) at the Ministry building of National Baby-sit Health Diplomacy (MNGHA) in SA (Enquiry protocol number - RC15/067).
Results
The socio-demographic characteristics of the AHT victims (northward=106) are shown in Table 1.
The mean historic period of the victims was vi.1 months and 52.viii% were male. More than three-quarters (84.9%) of participants lived with both parents, thirteen.1% with a single parent, and 2% with other relatives. Regarding parents' highest level of pedagogy, over half (58.ix%) had completed loftier schoolhouse education, followed past the college or higher degree (25.2%), and primary school or less (15.ix%). Amidst children who had experienced AHT, biological father was the perpetrator in 35.eight% of the cases, followed past biological mother (12.v%), step-father (xiv.3%), and step-mother (12.five%). In terms of health outcomes, over a quarter (26.four%) of the victims were either disabled or died.
Over the xi-year period, at that place was a sharp increase in the number of AHT cases, specifically later on 2014, from seven cases per twelvemonth in 2010 to xvi cases in 2020 (Figure one).
The yr-to-yr variation in AHT rates is shown in Figure ii.
AHT rates were calculated from child population data ranging from ii.4 to five.three per million population betwixt 2010 and 2020 which indicate that AHT rates varied widely from year to year. Figure iii shows the age distribution in months for AHT cases across the study population.
AHT affects predominantly children aged 0-12 months (72.half-dozen%), followed by 13-24 months (17.9%), 25-36 months (3.8%), 37-48 months (3.viii%), and 49-60 months (1.ix%). Victims of AHT were characterized past a predominance of crying infants (23.vi%), past history of abuse (thirteen.ii%), a child's chronic disease and disability (vii.6%), and prematurity (ii.eight%). Amidst the 106 cases, the suspected perpetrators of AHT incidents were the young aged parents (13.2%; Table 2).
Discussion
AHT results in severe injuries to the skull and intracranial contents and represents a significant affliction burden in infants and children. To the best of our noesis, this hospital-based kid protection center retrospective study is the first published report in SA amongst infants and children which reports rates of AHT over the last decade and characteristics of the children and their families. Our study results have 3 major findings. First, a large proportion of AHT victims identified were infants and males. Second, an increment in the number of AHT cases was found from year to twelvemonth. Third, crying infants were the main victims of AHT.
AHT is largely restricted to infants and males. Children anile <1 year are more likely to suffer brain injuries usually caused by CM than accidents [19]. Results from our study are consistent with those of Parks et al. who reported most children who accept fatal AHT aged <12 months and are males [12]. In Republic of estonia, Talvic et al. plant that all of the 26 AHT cases that were discovered and diagnosed between 1997 and 2003 were <1 yr [sixteen]. A study conducted in Turkey stated that 88% of all AHT cases were nether the age of two years and males represented 56% of the cases [20]. According to Frasier [21], the increased vulnerability may be related to infants' shut contact with their caregivers and need constant care as compared with older children. In addition, infants' heads are comparatively larger and encephalon is proportionately heavier for their body. Their neck muscles are not strengthened, since the ability to sustain the head upright develops from ii to 4 months [22]. Prevention strategies for AHT involve educational actions for parents of newborns before discharge from the infirmary which include videos and pamphlets disclosing the risks of AHT, the pattern of crying, and the strategies that parents can utilize when they feel frustrated with the crying babe might reduce the incidence of AHT among male person infants [23]. Dias et al. also revealed a decrease in AHT using written and video content about the consequences of shaking in addition to asking parents to voluntarily sign a commitment statement acknowledging receipt and agreement of the information [24].
Consistent with Kelly et al. report [25], we found an increment in the incidence of AHT over time. In some other written report, AHT rates from hospital discharge information ranged from 25.0 to 44.ix per 100,000 person-years between 2000 and 2011 [26]. These rates might be underestimated every bit many cases are non recognized as having been caused by CM or practice not come to the attention of wellness care providers to exist identified [12,21]. Pediatricians should conduct a thorough and objective medical evaluation of the babies with clinical features of potential AHT. They should consider consulting a physician specialized in CM to ensure the accuracy of the diagnosis. They should empathise that legal burdens of proof are not required for the diagnosis. They are required to report suspected CM to child protective services if a final diagnosis of CM has been fabricated or not. Every bit mandated reporters, they conduct the burden of recognizing and responding to medical manifestations of AHT [27].
Crying is an important mode of communication for babies that plays an important role to ensure survival, health, and development when they depend on their caregivers [23]. Although crying is normal for the initial period of their life, previous studies have reported that specific crying backdrop can cause frustration and stress for the caregivers, the stimulus that contributes to the occurrence of AHT [28]. Adamsbaum et al. have indicated that crying was the reported stimulus in 63% of the cases that was comparable to Flaherty'due south study where in 67% of confessions, crying was the circumstance that triggered the maltreatment [29,xxx]. However, our study reported that only 23.6% of crying infants were the main victim of AHT. It is anticipated that lack of consistency in the prevalence rate was due to knowledge and perception of different crying properties that contribute to the occurrence of AHT. There is an urgent demand for a meta-analysis of all available manufactures to explore the phenomenon among infants. The prevention programs demand to combine the understanding of specific properties of crying during the initial catamenia of a infant's life, the occurrence of inconsolable crying during their development, and the negative bear upon of crying during this period is the occurrence of AHT and other types of CM [28]. A universal AHT prevention program, the Period of Regal Crying, the objectives of which are to support caregivers in their understanding of early on increased crying in infancy and to reduce the incidence of AHT [26]. According to Dias et al. [24], information technology has been hypothesized that this intervention would reduce AHT by l% from a previously determined baseline. This intervention program can be recommended for caregivers in SA and should exist customized and implemented.
The study has some limitations. First, this is a retrospective review of a registry database that does not capture comprehensive data on the AHT. 2nd, the AHT cases are the selected sample from the emergency department. The sample does not include those who died of AHT before they were admitted to the infirmary. Therefore, the results may non represent the number of infants/children in the community. Third, the retrospective information obtained were limited to the quality of the documentation in the medical tape. Quaternary, this study cannot establish a causal relationship.
Conclusions
The results of this report indicate that AHT cases increment over fourth dimension in SA and need more attention of the health care providers, kid protection workers, counselors, constabulary enforcement personnel, and policy makers. Prevention and detection of AHT should exist priority in terms of hereafter management. Preventive measures need to focus on caregivers of the babies. Different training and educational programs need to be performed to heighten awareness of AHT. Enacting the pediatrician's mandatory reporting law will ameliorate the rate of reporting AHT cases. Future studies are required to accost the effect of AHT in the context of local culture.
References
- Al-Mahroos F, Al-Amer E, Al-Hashimi H, Abdulla A, Hameed Due north: Abusive caput trauma in children: the extent and clinical characteristics. Bahrain Med Message. 2011, 33:174-178.
- Child maltreatment: factsheet. (2007). Accessed: May 10, 2021: http://www.cdc.gov/ncipc/factsheets/cmfacts.htm.
- Keenan HT, Runyan DK, Marshall SW, Nocera MA, Merten DF, Sinal SH: A population-based study of inflicted traumatic brain injury in young children. JAMA. 2003, 290:621-6. ten.1001/jama.290.five.621
- Hennes H, Kini N, Palusci VJ: The epidemiology, clinical characteristics and public health implications of shaken baby syndrome. The Shaken Infant Syndrome: A Multidisciplinary Arroyo. Lazoritz S, Palusci VJ (ed): Haworth Maltreatment & Trauma Press, Binghamton; 2001.
- Makaroff KL, Putnam FW: Outcomes of infants and children with inflicted traumatic encephalon injury. Dev Med Child Neurol. 2003, 45:497-502. x.1017/s0012162203000926
- Instance MD: What Does Science Tell Us Most Abusive Head Trauma in Infants and Young Children?. National Center on Shaken Infant Syndrome, Farmington; 2021.
- Baeesa S, January Yard: The shaken infant syndrome. Saudi Med J. 2000, 21:815-820.
- Xiang J, Shi J, Wheeler KK, Yeates KO, Taylor HG, Smith GA: Paediatric patients with calumniating head trauma treated in U.s.a. Emergency Departments, 2006-2009. Brain Inj. 2013, 27:1555-61. x.3109/02699052.2013.831126
- Shanahan ME, Zolotor AJ, Parrish JW, Barr RG, Runyan DK: National, regional, and land calumniating head trauma: application of the CDC algorithm. Pediatrics. 2013, 132:e1546-53. 10.1542/peds.2013-2049
- Liley Due west, Stephens A, Kaltner One thousand, Larkins S, Franklin RC, Tsey Thou: Infant abusive head trauma -incidence, outcomes and awareness. Aust Fam Md. 2012, 41:823-826.
- Bruce DA, Zimmerman RA: Shaken impact syndrome. Pediatr Ann. 1989, xviii:482-4, 486-9, 492-4. ten.3928/0090-4481-19890801-07
- Parks SE, Kegler SR, Annest JL, Mercy JA: Characteristics of fatal abusive head trauma amidst children in the The states: 2003-2007: an awarding of the CDC operational case definition to national vital statistics data. Inj Prev. 2012, xviii:193-9. x.1136/injuryprev-2011-040128
- Frasier LD, Kelly P, Al-Eissa M, Otterman GJ: International issues in calumniating head trauma. Pediatr Radiol. 2014, 44 Suppl 4:S647-53. 10.1007/s00247-014-3075-0
- Myhre MC, Grøgaard JB, Dyb GA, Sandvik 50, Nordhov M: Traumatic head injury in infants and toddlers. Acta Paediatr. 2007, 96:1159-63. 10.1111/j.1651-2227.2007.00356.x
- Tingberg B, Falk Ac, Flodmark O, Ygge BM: Evaluation of documentation in potential abusive head injury of infants in a Paediatric Emergency Section. Acta Paediatr. 2009, 98:777-81. x.1111/j.1651-2227.2009.01241.x
- Talvik I, Metsvaht T, Leito K, et al.: Inflicted traumatic brain injury (ITBI) or shaken baby syndrome (SBS) in Estonia. Acta Paediatr. 2006, 95:799-804. 10.1080/08035250500464923
- Al-Saadoon M, Elnour IB, Ganesh A: Shaken baby syndrome every bit a course of calumniating head trauma. Sultan Qaboos Univ Med J. 2011, 11:322-327.
- Kattan H: Child abuse in Saudi Arabia: written report of 10 cases. Ann Saudi Med. 1994, fourteen:129-33. 10.5144/0256-4947.1994.129
- Molina DK, Clarkson A, Farley KL, Farley NJ: A review of edgeless force injury homicides of children aged 0 to five years in Bexar County, Texas, from 1988 to 2009. Am J Forensic Med Pathol. 2012, 33:344-8. 10.1097/PAF.0b013e31821a88c4
- Yaylaci South, Dallar Y, Sayar Y, Tasar Chiliad, Tiras U, Tekin D: Calumniating head trauma in Turkey and affect of multidisciplinary team establishment efforts on instance finding and direction: preliminary findings. Eurasian J Emerg Med. 2016, xv:24-29. 10.5152/eajem.2016.52386
- Frasier LD: Abusive caput trauma in infants and young children: a unique contributor to developmental disabilities. Pediatr Clin North Am. 2008, 55:1269-85, vii. 10.1016/j.pcl.2008.08.003
- Joint statement on shaken baby syndrome. (2001). Accessed: December 12, 2020: http://world wide web.hc-sc.gc.ca/hppb /childhood-youth/cyfh/child_and_youth/physical_health/shaken_baby.html.
- Lopes NR, Eisenstein Eastward, Williams LC: Calumniating head trauma in children: a literature review. J Pediatr (Rio J). 2013, 89:426-33. x.1016/j.jped.2013.01.011
- Dias MS, Smith Chiliad, DeGuehery K, Mazur P, Li V, Shaffer ML: Preventing abusive caput trauma among infants and young children: a hospital-based, parent education program. Pediatrics. 2005, 115:e470-seven. x.1542/peds.2004-1896
- Kelly P, John Due south, Vincent AL, Reed P: Abusive head trauma and accidental head injury: a 20-year comparative report of referrals to a hospital child protection team. Arch Dis Child. 2015, 100:1123-thirty. 10.1136/archdischild-2014-306960
- Zolotor AJ, Runyan DK, Shanahan M, et al.: Effectiveness of a statewide abusive caput trauma prevention program in Due north Carolina. JAMA Pediatr. 2015, 169:1126-31. 10.1001/jamapediatrics.2015.2690
- Narang SK, Fingarson A, Lukefahr J: Abusive head trauma in infants and children. Pediatrics. 2020, 145:e20200203. 10.1542/peds.2020-0203
- Lee C, Barr RG, Catherine N, Wicks A: Age-related incidence of publicly reported shaken baby syndrome cases: is crying a trigger for shaking?. J Dev Behav Pediatr. 2007, 28:288-93. 10.1097/DBP.0b013e3180327b55
- Adamsbaum C, Grabar S, Mejean N, Rey-Salmon C: Abusive caput trauma: judicial admissions highlight fierce and repetitive shaking. Pediatrics. 2010, 126:546-55. 10.1542/peds.2009-3647
- Flaherty EG: Assay of flagman histories in abuse: comparing initial histories with subsequent confessions. Child Abuse Negl. 2006, 30:789-98. x.1016/j.chiabu.2005.12.008
Original article
peer-reviewed
Epidemiology of Abusive Head Trauma Among Children in Saudi Arabia
Ethics Statement and Disharmonize of Interest Disclosures
Human subjects: Consent was obtained or waived past all participants in this written report. King Abdullah International Medical Research Middle issued approval RC15/067. The study obtained ethical clearance from the Institutional Review Board (IRB) of the King Abdullah International Medical Inquiry Middle (KAIMRC) in Kingdom of saudi arabia. Hospital medical tape numbers were used without any identification cloth. The data were collected only for research purposes and were not used for other purposes. A serial of measures were taken to ensure the protection of confidentiality. The information did not contain the name of the patient but were labeled with a reconstructable personal alphanumeric identifier. All data were stored on a designated calculator with an access-limited locked hard drive. Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue. Conflicts of interest: In compliance with the ICMJE compatible disclosure grade, all authors declare the post-obit: Payment/services info: The authors would like to thank King Abdullah International Medical Research Centre (KAIMRC) for their fiscal support of this report with grant number - RC15/067. Financial relationships: Hassan Saleheen, Majid Al-Eissa, Fahad Alanazi, Mohammed Hamaid, Abdullah Alshamrani, Ahmed Alhuwaymani, Waleed Jarwan declare(south) a grant from King Abdullah International Medical Research Center (KAIMRC). Other relationships: All authors have declared that there are no other relationships or activities that could appear to accept influenced the submitted work.
Article Data
DOI
10.7759/cureus.19014
Cite this article as:
Alanazi F S, Saleheen H, Al-Eissa G, et al. (October 24, 2021) Epidemiology of Calumniating Caput Trauma Among Children in Saudi Arabia. Cureus 13(x): e19014. doi:10.7759/cureus.19014
Publication history
Peer review began: Oct xiii, 2021
Peer review ended: October 20, 2021
Published: October 24, 2021
Copyright
© Copyright 2021
Alanazi et al. This is an open access article distributed under the terms of the Creative Eatables Attribution License CC-By 4.0., which permits unrestricted employ, distribution, and reproduction in any medium, provided the original author and source are credited.
License
This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Original article
peer-reviewed
Epidemiology of Abusive Caput Trauma Among Children in Kingdom of saudi arabia
Figures etc.
Source: https://www.cureus.com/articles/73756-epidemiology-of-abusive-head-trauma-among-children-in-saudi-arabia


0 Response to "Wisconsin Shaken Baby Syndrome What Percent of Perpetrators Are Male"
Post a Comment